Gastro-Enterology
Introduction
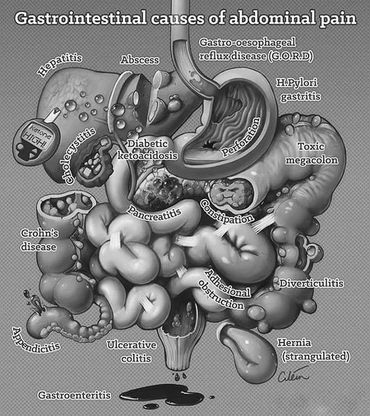
Gastroenterology is the study of the esophagus, stomach, small intestine, colon and rectum, pancreas, gallbladder, bile ducts, and liver. Its main field of research and study is the normal function and diseases of these organs.
A gastroenterologist requires a detailed understanding of the natural anatomy of all of the organs mentioned above as well as motion through the intestines and gastrointestinal tract to maintain healthy digestion and absorption of food intake, waste removal, and metabolic processes.
The doctors practicing this medicinal branch are called gastroenterologists. Generally, they have undergone approximately eight years of pre-medical and medical training, a year-long internship (if not part of the specialty), three years of internal medicine residency, and two or three years in the practice of gastroenterology.
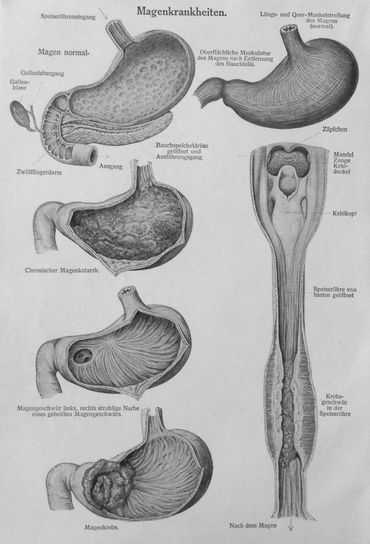
A gastroenterologist must also have a clear understanding of the diseases that damage the digestive system's organs, such as:
- peptic ulcer disease
- gastric cancers
- esophageal cancers
- achalasia
- Barret's esophagus
- colon polyps
- colon and bowel cancers
- pancreatitis
- pancreatic cancers
- cholecystitis
- biliary tract disease
- gallbladder stones and cancer
- hepatitis
- gastroesophageal reflux
- colitis
- nutritional problems and malabsorption,
- Irritable Bowel Syndrome (IBS)
- a host of other disease conditions

Historical Records of Internal Medicine
In the following presentation, we aim at presenting the stomach and bowel physiology from a historical perspective.
We exert adequate information on how the ancients interpreted digestive processes and how they wanted to adjust them to the dominating humoral theory of disease and correspondingly as medicine progressed through the ages.

History
Long before man entered history, the first medical agent had appeared. There is no denying that food intake is correlated with the emergence of the first drug. Early man, eating vegetables, spices, and roots, felt shocked, exhausted, and fell asleep; may also have vomited or suffered from diarrhea and acute diseases, some of which may had fatal consequences. Food agents have become medicines at some point.
Since old times, shamans have mostly believed that the seats of unique spiritual forces are governed by specific organs.
These hidden forces are mystically controlling the processes of the body.
There are numerous testimonials to gastrointestinal mechanisms, digestive system anatomy, food status and sense, and spiritual procedures that applied to nourishment in one of the oldest papyruses (particularly Ebers papyrus). Abundant references we also find in the Bible's sacred pages, in ancient Chinese and Indian medical papers, and notably in the classical manuscripts of Greek and Roman physicians.
Erasistratos from Keos (around 310-250 B.C.) outlined the premise that blood is extracted from nutrition after it has been fragmented into valuable and useless components. Then food combined with blood goes to the heart's right chamber and is used to sustain the lungs.
Blood is further transferred through arteries to feed the majority of the body.
Galen later accepted this idea.
The first founder of the whole practical philosophy of the human body structure was Claudius Galen (around 130-200), who lived at the end of ancient times and decided to conduct the approach on the humor of Hippocrates.
Galen believed that digestion starts in the stomach, where the first food is dissolved.
Then, due to the pumping power of the arteries, and with the aid of "pneuma psychicon" and human heat, it travels to the intestine where it is decomposed and then transferred to the liver through the vessels.
Passing through the liver, food is converted into blood, pumped into the hepatic vein, and further into the heart through the lower caval vein.
Galen assumed the blood level to be equal to the food intake.
The theory lasted until the Renaissance.
Galen's concept of the production of body fluids as brewing processes and "chemical boiling" of raw or fermented foods ("apepsis") survived, however, until the early days of the 17th century iatrochemical school.
Early digestive issues became primarily linked to gastrointestinal disorders, effects of "poor" systemic fluids (depending on the school - pneuma or archeus) or even having one's vital forces possessed by the devil.
Due to the lack of accurate medical information, the inability to recognize and diagnose diseases and provide surgical treatment, physicians only used herbs to handle gastrointestinal problems.
In acute diseases with symptoms such as colic pain, vomiting, diarrhea, melaena, constipation, and flatulence, herbs were likely to be used.
In the books of great Arab doctors of the close of our era's first millennium, one might better understand such. Both Razes (about 850-923) and particularly Avicenna (980-1037) adopted the teachings of Galen, and it is challenging to find their original principles of physiology and digestive pathology.
Paracelsus (1443-1541) first had a reasonable attitude towards the pharmacological side of the internal disease, including gastrointestinal problems. He was from Switzerland, and at the turn of the Middle Ages and the Renaissance, he became the most excellent physician.
He first established the idea that illness is a natural phenomenon related to the human body. He believed this arose from several factors such as a low standard of living, unhealthy behavior, an inadequate diet, particularly interesting facts.
So, according to the doctrine of the signatures, he suggested dietary prescription using natural plant medicines. According to this definition, failure organs should be treated with plants that visually resemble them, e.g., yellowish saffron leaves should be used to treat jaundice or liver diseases.

Erasistratos from Keos (around 310-250 B.C.)

Claudius Galenus Greek: Κλαύδιος Γαληνός (129 AD – c. 200/c. 216)

Paracelsus ( 1493/4 – 24 September 1541), born Theophrastus von Hohenheim (full name Philippus Aureolus Theophrastus Bombastus von Hohenheim

Introduction to Modern Gastro-enterology
At the beginning of the 19th century, medical studies addressed the roles of the stomach and its chyme. American physicist William Beaumont (1785-1853), a student at the prestigious London and Edinburgh Universities, was a pioneer of this movement.
He worked on the American-Canadian border at the Army Hospital in Fort Mackinok.
One day, a patient with an abdominal gunshot wound with the fistula of the stomach was taken to the hospital.
Beaumont, considered to be an excellent surgeon, healed the wound leaving - the stomach fistula - with the patient's consent.
The reality allowed him to study the interior of the stomach for several years and examine its contents.
Beaumont initiated the first modern studies in digestion physiology in July 1822.
These succeeded in isolating the hydrochloric acid from the stomach juice, finding the link between the stomach secretion and psychological changes, and the first attempt to explain the motility of the stomach.
His short book The Physiology of Digestion (Beaumont W. Experiments and Observations on the Gastric Juice and the Physiology of Digestion, Plattsburg 1833. ) was a groundbreaking piece of scientific gastrology.
Beaumont's discovery of hydrochloric acid as the main ingredient in stomach juice was confirmed at the meeting of the Royal Society in London on 11 December 1823 by a physician from London's Gray Hospital – William Prout (1785-1850).
He had found many forms of hydrochloric acid in the stomachs, e.g., dogs, rats, goats, cats, hares, and, of course, in humans. In his great work On the Origin of Acid and Saline Matters, shortly published in 1823, he described these data. ( Prout W. On the Application of Chemistry to Physiology, Pathology, and Practice. Medical Gazette 1831; 8: 257-265)
The foundations of the completely new physiological school were established in the 19th century. This occurred partly thanks to the support of French and German scientists linked to the biggest schools and institutes in those days.
The new French physiological school was founded by François Magendie (1783-1855), professor of pathology at the College de France, and the best pupil of the colossal pathologist-Xavier Bichat.
He was a member of the group of people opposed to the theory of vitalism.
To him, biological processes are simply physical and chemical responses happening in the body.
He was not only interested in morphological or stable features of pathogens, including being a pathologist.
He was the first to establish and explain illness and clinical effects on animal models.
These investigations made him the author of the modern trend-experimental physiology.
Concerning the field of gastrointestinal tract physiology, in 1813, he gave a detailed explanation of the mechanism of swallowing and vomiting and in 1844, showed (in unpublished data) that food first digested in the intestine was transmitted through the portal vein into the liver.
The most outstanding French physiologist was Claude Bernard (1813-1878), a student of Magendi, known as the creator of modern physiology.
He first became a professor of physiology at the Parisian Sorbona and then took over the Department of Physiology at the College de France after his boss. Bernard was the experiment's undisputed master.
He discovered a variety of biological anomalies during his lifetime. He established new organic paths, such as the study of endocrine secretion, neurophysiology, laboratory technique, and experimental pharmacology, that quickly became new medical fields.
He discovered the liver's ability to synthesize and accumulate glycogen by studying its physiological function.
In 1849 he administered the first insulin injection into the fourth brain chamber (so-called Claude Bernard injection), causing the sugar blood level to rise rapidly and dramatically, culminating, as he believed in spontaneous glycogenolysis in the liver.
This observation has become the foundation of the theory that all glands secrete certain particular substances directly into the blood in addition to the normal secretion. Such processes he identified as endocrine secretion in the dissertation submitted to the Faculty of Sciences in 1853 on the role of the liver (Bernard C. Recherches sur une nouvelle fonction du foie considéré comme organe producteur de matiere sucrée chez l'homme et les animaux, Paris 1853)
Historical work into the enzymatic roles of the liver and pancreas and the digestive system of the pancreas (1856) form part of his very impressive achievements. ( Bernard C. Mémoires sur le pancréas et sur le rôle du suc pancréatique dans les phénomenes digestifs, particulierement dans la digestion des matieres grasses neutres, Paris 1856)
He was very interested in anatomy, histology, embryology, anthropology, biology as well as philosophy and philology besides his disciplines. He wrote his works in Latin, German, Czech, and Polish.
He was the founder of the first experimental physiology institute in which he conducted groundbreaking studies in physiology and cytophysiology in his most significant discoveries, e. g — conducting fibers of the heart denominated after him.
All the best physiologists came from Purkynì school during the first half of the 19th century. Johannes Müller, Karl Ludwig, Herman Helmholtz were among them.

William Beaumont (November 21, 1785 – April 25, 1853)

François Magendie (1783-1855)
Claude Bernard (1813-1878)

Johannes Müller(1801 - 1858 )

Carl Friedrich Wilhelm Ludwig (29 December 1816 – 23 April 1895)

Hermann Ludwig Ferdinand von Helmholtz (August 31, 1821 – September 8, 1894

Karl Ludwig (1816-1895) set the greatest achievements in the field of gastrointestinal tract physiology. ( Schroer H. Carl Ludwig. Begründer des messenden Experimentalphysiologie 1816-1895, Stuttgart 1967 (publications pp. 294-312).
Other notable German physiologists of the late 19th century were Ernst von Brücke (1819-1892) and Rudolph Heidenhain (1834-1897), professor of physiology at the University of Breslau.
Von Brücke had isolated the pure pepsin at the end of his carrier.(Lesky E. Die Wiener Medizinische Schule im 19. Jahrhundert in Studien zur Geschichte der Universität Wien, part VI Graz, Cologne 1965 p. 258)
-the most important von Brücke's works and the most important secondary literature -
This was one of those landmarks that launched the era of modern medical diagnostics. Heidenhain, who focused on the role of endocrine glands at the beginning of his carrier in 1866, found that secretion often induces structural gland changes.
Examining gastric secretion in 1878, he identified and described three types of cells in gastric mucosa: chief or zymogenic cells releasing pepsin, hydrochloric acid-secreting parietal cells, and epithelial cells.
(Grützner P. Pfl. Arch 1898; 72: 263-265 (collected works of Heidenhain).
A Polish scientist-Jagiellonian University professor-Walery Jaworski (1849-1924) made a significant discovery in 1889. This.was the identification of the circular, rod bacterium, which is typical of cancer of the stomach and ulcer disease .(Jaworski W. Podrêcznik chorób ¿o³¹dka i dyjetetyki szczegó³owej (Handbook of Gastric Diseas and Dietetics), Kraków 1889 p. 33)

Ernst Wilhelm Ritter von Brücke (6 July 1819 – 7 January 1892)
Rudolph Heidenhain (1834-1897)
Photo Gallery





References & Citations
THE SHORT HISTORY OF GASTROENTEROLOGY
http://www.jpp.krakow.pl/journal/archive/12_03_s3/pdf/9_12_03_s3_article.pdf
1.Beaumont W. Experiments and Observations on the Gastric Juice and the Physiology of Digestion, Plattsburg 1833.
2.Prout W. On the Application of Chemistry to Physiology, Pathology, and Practice. Medical Gazette 1831; 8: 257-265.
3.Bernard C. Recherches sur une nouvelle fonction du foie considéré comme organe producteur de matiere sucrée chez l'homme et les animaux, Paris 1853.
4.Schroer H. Carl Ludwig. Begründer des messenden Experimentalphysiologie 1816-1895, Stuttgart 1967 (publications pp. 294-312.
5.Lesky E. Die Wiener Medizinische Schule im 19. Jahrhundert in Studien zur Geschichte der Universität Wien, part VI Graz, Cologne 1965 p. 258 (the most important von Brücke's works and the most important secondary literature.
6.Grützner P. Pfl. Arch 1898; 72: 263-265 (collected works of Heidenhain
7.Jaworski W. Podrêcznik chorób ¿o³¹dka i dyjetetyki szczegó³owej (Handbook of Gastric Diseas and Dietetics), Kraków 1889 p. 33
Gastroenterology principles
The digestive tract provides a continuous supply of water, electrolytes, vitamins, and nutrients to the body.
This requires the movement of food through the food tract; the secretion of digestive juices and the digestion of food; the absorption of water, various electrolytes, vitamins, and digestive products; the circulation of blood through the gastrointestinal organs to remove the absorbed substances; and the control of all these functions through local, nervous and hormonal systems.
Each part is adjusted to its specific functions: some for simple passage of food, such as the esophagus; others for the temporary storage of food, such as the stomach; and others for digestion and absorption, such as the small intestine.
Neural Control of Gastrointestinal Function—Enteric Nervous System
The gastrointestinal tract has its nervous system, entitled as the enteric nervous system. This resides solely in the gut wall, beginning in the esophagus and spreading to the anus all the way. In this enteric network, the number of neurons is about 100 million, almost the same as in the whole spinal cord.
When monitoring gastrointestinal movements and secretion, this highly developed enteric nervous system is particularly important.
The enteric nervous system consists primarily of two plexuses,- an external plexus located between the longitudinal and circular layers of muscle, called the myenteric plexus or Auerbach's plexus, and an internal plexus, called the submucosal plexus or Meissner's plexus, lying in the submucosa.
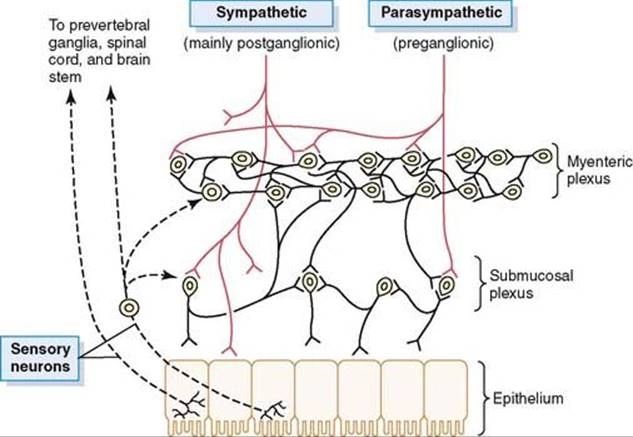
This figure depicts the neural regulation of the intestinal wall, displaying (1) myenteric and submucosal plexuses (black fibers); (2) extrinsic control of these plexuses by sympathetic and parasympathetic nervous systems (red fibers); and (3) sensory fibers from the luminal epithelium and intestinal wall to enteric plexuses, then to the spinal cord prevertebral ganglia and then to the spinal cord and brain stem.
The myenteric plexus primarily controls gastrointestinal activities, while the submucosal plexus mainly regulates gastrointestinal secretion and systemic blood flow.
The myenteric plexus primarily controls gastrointestinal activities, while the submucosal plexus mainly regulates gastrointestinal secretion and systemic blood flow.
Note the extrinsic sympathetic and parasympathetic fibers that attach with both the myenteric and submucosal plexuses, particularly in this figure.
Although the enteric nervous system can act independently of these extrinsic nerves, activation by parasympathetic and sympathetic mechanisms can significantly enhance or impede gastrointestinal functions.
This diagram also indicates the sensory nerve endings which stem in the gastrointestinal epithelium or gut wall and transmit afferent fibers to both entrance plexuses, as well as (1) to the sympathetic nervous system prevertebral ganglia, (2) to the spinal cord, and (3) to the brain stem in the vagus nerves. Such sensory nerves may generate specific reflexes within the gut wall itself, as well as other reflexes transmitted to the gut either from the prevertebral ganglia or from the basal regions of the brain.
Differences Between the Myenteric and Submucosal Plexuses
Most of the myenteric plexus consists of a linear chain of many interconnecting neurons that stretches the gastrointestinal tract's entire length.
The diagram displays a portion of this chain.
Because the myenteric plexus stretches throughout the intestinal wall and because it sits between the longitudinal and circular layers of the intestinal smooth muscle, it is mainly concerned with regulating muscle activity along the length of the intestines.
When this plexus is stimulated the main effects are (1) increased tonic contraction, or tone of the gut wall; (2) increased rhythmic contraction intensity; (3) slightly increased rate of contraction; and (4) increased speed of conduction of stimulating waves along the gut wall, resulting in rapid acceleration of the peristaltic gut waves.
Because some of its neurons are inhibitory, the myenteric plexus should not be considered entirely excitatory; its fiber-endings secrete an inhibitory transmitter, probably vasoactive intestinal polypeptide, or some other inhibitory peptide. The subsequent inhibitory impulses are particularly useful for inhibiting some of the intestinal sphincter muscles that hinder the passage of food along consecutive gastrointestinal tract sections, such as the pyloric sphincter, which regulates the emptying of the stomach into the duodenum, and the ileocecal valve sphincter, which controls the emptying from the small intestine into the cecum.
An Introduction to Common Symptoms & Signs in Gastroenterology
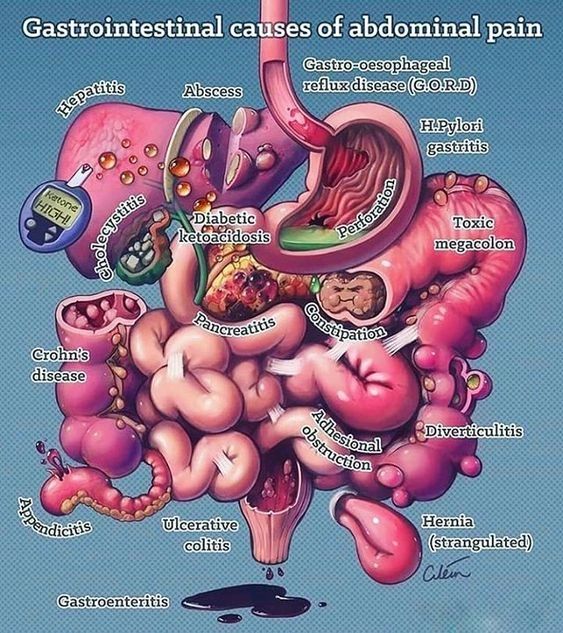
Symptoms and disorders of the gastrointestinal (GI) are widespread in the population at large.
All doctors, regardless of specialty, will encounter GI symptoms and disease. Therefore, providing a system to treat specific GI issues is essential for all physicians.
Conducting a thorough background is the key to diagnosis and successful treatment, particularly for people with GI symptoms. The first goal in trying to apprehend records is to not neglect serious illness, such as GI malignancy.
It is necessary to look for so-called "warning signs." Dysphagia, GI bleeding, significant weight loss, fatigue, and sleep-waking discomfort are indicators of emergency call symptoms that should cause an immediate examination to exclude a severe GI deficiency.
Recognizing that symptoms of GI can indicate organic disease or functional disease is essential. Organic illness refers to a well-defined condition (such as peptic ulcer disease, inflammatory disease of the stomach, or malignancy).
It is more prevalent for patients with functional GI disorders. They have symptoms, but on physical examination or diagnostic testing, they have no objective abnormality. Irritable bowel syndrome (IBS) and functional dyspepsia (FD) are the most severe of these conditions. When separating natural from active infection, the carefully chosen past is often useful.
The accurate description of the condition will include a thorough consultation.
These would cover starting time ( onset ), location or position, duration, individual characteristics, and radiation. It is essential to look for aggravating or relieving causes (e.g., feeding or defecation), the examination of other GI signs, past history of GI illness or other conditions, recent surgery, and family history of GI disease.
For several reasons, psycho-social history is essential. For patients with a history of traumatic life experiences, the functional disorder is more severe.
Anxiety or psychological stress may intensify symptomatology (e.g., inflammatory bowel disease) in clinicians with organic illness. Such a background is also essential to address the questions of the patient.
If a physician does not know what they are, he or she can not adequately address the issues of a patient.
References & Citations
https://doctorlib.info/physiology/textbook-medical-physiology/62.html
Bibliography
Adelson D.W., Million M. Tracking the moveable feast: sonomicrometry and gastrointestinal motility. News Physiol Sci. 2004;19:27.
Daniel E.E. Physiology and pathophysiology of the interstitial cell of Cajal: from bench to bedside. III. Interaction of interstitial cells of Cajal with neuromediators: an interim assessment. Am J Physiol Gastrointest Liver Physiol. 2001;281:G1329.
Grundy D., Al-Chaer E.D., Aziz Q., et al. Fundamentals of neurogastroenterology: basic science. Gastroenterology. 2006;130:1391.
Hobson A.R., Aziz Q. Central nervous system processing of human visceral pain in health and disease. News Physiol Sci. 2003;18:109.
Holst J.J. The physiology of glucagon-like peptide 1. Physiol Rev. 2009;87:1409.
Huizinga J.D. Physiology and pathophysiology of the interstitial cell of Cajal: from bench to bedside. II. Gastric motility: lessons from mutant mice on slow waves and innervation. Am J Physiol Gastrointest Liver Physiol. 2001;281:G1129.
Huizinga J.D., Lammers W.J. Gut peristalsis is governed by a multitude of cooperating mechanisms. Am J Physiol Gastrointest Liver Physiol. 2009;296:G1.
Jeays A.D., Lawford P.V., Gillott R., et al. A framework for the modeling of gut blood flow regulation and postprandial hyperaemia. World J Gastroenterol. 2007;13:1393.
Johnson L.R. Gastrointestinal Physiology, ed 3. St. Louis: Mosby, 2001.
Kim W., Egan J.M. The role of incretins in glucose homeostasis and diabetes treatment. Pharmacol Rev. 2009;60:470.
Kolkman J.J., Bargeman M., Huisman A.B., Geelkerken R.H. Diagnosis and management of splanchnic ischemia. World J Gastroenterol. 2008;14:7309.
Lammers W.J., Slack J.R. Of slow waves and spike patches. News Physiol Sci. 2001;16:138.
Moran T.H., Dailey M.J. Minireview: Gut peptides: targets for antiobesity drug development? Endocrinology. 2009;150:2526.
Nauck M.A. Unraveling the science of incretin biology. Am J Med. 2009;122(Suppl 6):S3.
Powley T.L., Phillips R.J. Musings on the wanderer: what’s new in our understanding of vago-vagal reflexes? I. Morphology and topography of vagal afferents innervating the GI tract. Am J Physiol Gastrointest Liver Physiol. 2002;283:G1217.
Phillips R.J., Powley T.L. Innervation of the gastrointestinal tract: patterns of aging. Auton Neurosci. 2007;136:1.
Sanders K.M., Ordog T., Ward S.M. Physiology and pathophysiology of the interstitial cells of Cajal: from bench to bedside. IV. Genetic and animal models of GI motility disorders caused by loss of interstitial cells of Cajal. Am J Physiol Gastrointest Liver Physiol. 2002;282:G747.
Schubert M.L., Peura D.A. Control of gastric acid secretion in health and disease. Gastroenterology. 2008;134:1842.
Vanden Berghe P., Tack J., Boesmans W. Highlighting synaptic communication in the enteric nervous system. Gastroenterology. 2008;135:20.
First Principles of Gastroenterology and Hepatology
A. B. R. Thomson and E. A. Shaffer, Editors
Chapter 1: Common Symptoms and Signs in Gastroenterology N. Saloojee With sections authored by: R.F. Bursey, M.C. Champion, C. Dube, J.M. Fardy, S. Grégoire, D.G. MacIntosh, D.G. Patel, A. Rostom, N. Saloojee, L.J. Scully, A.S.C. Sekar, W.G. Thompson and J.M. Watters
Copyright © 2019 Louisiana Agriculture Preservation Society - All Rights Reserved.
Powered by GoDaddy Website Builder